These findings highlight how racial discrimination can negatively impact health, says coauthor Negar Fani, PhD, an associate professor of psychiatry and behavioral sciences at the Emory University School of Medicine in Atlanta.
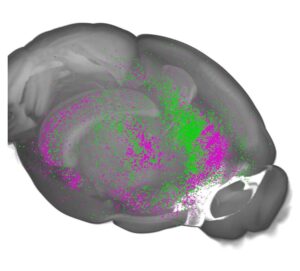
“We were able to show there’s increased engagement in a brain network associated with rumination in relation to racism, and it has a link to accelerated aging. This helps us better understand the link between why racial discrimination is so frequently associated with more health problems,” says Dr. Fani.
Rumination means thinking over and over again about something you’ve experienced, perhaps trying to analyze it in different ways, she explains.
“We all engage in rumination; it’s a very natural process. But sometimes rumination keeps us stuck in a loop, and it can wear down the brain over time,” she says.
Even ‘Subtle’ Racism Can Have Negative Health Impacts
“Racism is one of the most debated topics in our culture right now. I think it’s such a polarizing term,” says Fani.
Racism can be overt, but it can also be very subtle, says Fani.
“Examples can be as slight as saying, ‘Oh, you speak so articulately,’ or a behavior like a woman clutching her purse as a Black man is walking down the street. The person on the receiving end of it might not even react when they experience racism, but it’s a very real thing,” she says.
Black Americans experience injustice, hostility, and inequitable treatment based on their skin color, race, and ethnicity. These negative experiences occur in many situations, from medical settings, to education, to trying to get a job or buy a house.
Accelerated Aging May Increase the Risk of Diabetes, Dementia and Heart Disease
To explore how Black women’s experience of racism impacts different areas of the brain, researchers recruited 90 Black women who were 38 years old on average from the Grady Trauma Project, a community-based initiative investigating trauma-related disorders.
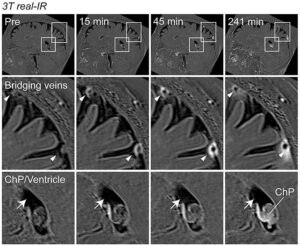
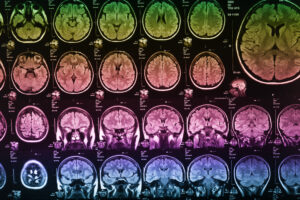
Participants underwent assessments for racial discrimination, trauma exposure, and post-traumatic stress disorder (PTSD) symptoms. Information about brain activity was collected via MRI, and information on aging was determined using blood samples.
“There are certain blood-based biomarkers that indicate the difference between our cellular age and our actual age, which gives us an index of an accelerated rate of aging,” says Fani.
The analysis revealed a relationship between discrimination and accelerated aging by way of higher engagement in this rumination network in the brain, she says.
“People who have had more racist experiences ruminate more, and we think that over time, this is affecting biological aging. We’re meant to age at a particular rate, and when we accelerate that rate of aging, we’re more likely to experience diseases associated with aging — including diabetes, heart disease, strokes, and dementia — earlier in life,” says Fani.
These findings could be part of the reason that Black Americans have much higher rates of these aging-related diseases, and develop them at much earlier ages, she says.
Black Americans Twice as Likely to Develop Dementia and Alzheimer’s Compared With Their White Peers
This study helps further the understanding of how racism impacts the health of Black Americans, says Michelle Mielke, PhD, a professor of epidemiology and prevention, and researcher at the Wake Forest University School of Medicine in Winston-Salem, North Carolina.
“Alzheimer’s disease and related dementias are much more prevalent in Black Americans compared with white Americans, and there’s been a lot of work going on lately trying to understand why that is,” says Dr. Mielke, who was not involved in this study.
While some studies have shown that racial discrimination is associated with poor cognitive outcomes or dementia, the mechanisms by which it occurs are not yet known, she says.
These findings are a big step forward because they are actually using MRIs and blood biomarkers to understand the specific effects of racial discrimination on the brain and the role of biological aging that may be contributing to the increased risk of Alzheimer’s disease and related dementias, says Mielke.
Researchers plan to continue exploring the psychological processes outside a lab setting to understand what happens to people in response to a racist threat or experience, and what happens when they are ruminating about those experiences.
Racism Should Be Assessed in Primary Care Settings
Fani believes these findings continue to build a case for screening for racism in a medical setting.
“Just like we screen for factors such as family history or psychiatric issues like depression, I think screening for the experiences of racism could be an important tool in identifying people at risk for certain health conditions,” she says.
“It’s being shown in so many different ways. This is something that’s linked to worse health outcomes. Why not include it in primary care settings as an assessment measure to see if people are at higher risk when they report more frequent experiences?” she says.
Beyond the medical community, organizations and businesses can support implicit bias training on a mandatory basis, says Fani.
This could help reduce some of the manifestations of implicit bias, especially when people aren’t intending to discriminate against someone else, but it comes across that way. Implementing mandatory trainings could help people see their blind spots and educate them to understand how not to engage in behaviors that others perceive as discriminatory, she says.





Post Comment