Acetaminophen shows promise in warding off acute respiratory distress syndrome, organ injury in patients with sepsis
Findings from NIH-supported clinical trial suggests the drug has the greatest benefit in the sickest patients.
A National Institutes of Health (NIH)-supported clinical trial has found that intravenous acetaminophen reduced sepsis patients’ risk of having organ injury or developing acute respiratory distress syndrome, a serious condition that allows fluid to leak into the lungs. Sepsis is the body’s uncontrolled and extreme response to an infection. While the trial did not improve mortality rates in all patients with sepsis regardless of severity, the researchers found that acetaminophen gave the greatest benefit to the patients most at risk for organ damage. With the therapy, those patients needed less assisted ventilation and experienced a slight, though statistically insignificant, decrease in mortality. The study published in JAMA.
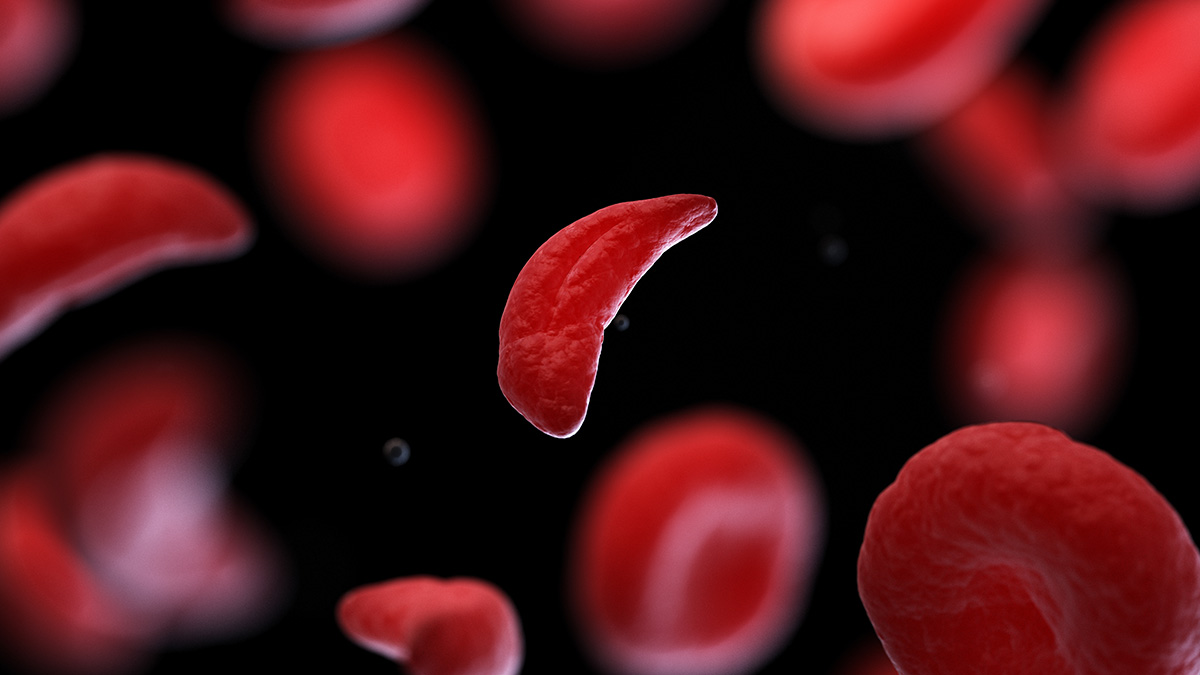
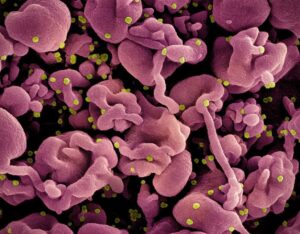
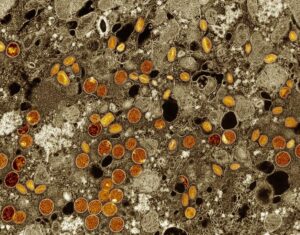
In sepsis, red blood cells become injured and die at abnormally high rates, releasing so called “cell-free hemoglobin” into the blood. The body becomes overwhelmed and can’t remove this excess hemoglobin which can lead to organ damage. Previous work from Lorraine Ware, M.D., professor of medicine, pulmonary and critical care at Vanderbilt University, Nashville, Tennessee, and the first author of the current study showed that acetaminophen, in addition to relieving pain and reducing fevers, had been shown to block the harmful effects of cell-free hemoglobin on the lungs, which are at major risk of injury during sepsis. Limited research had also suggested that acetaminophen might work better for patients with the most severe sepsis – those with higher levels of cell-free hemoglobin, which have been linked to a greater risk of developing acute respiratory distress syndrome and a higher risk of death.
Scientists note that identifying high levels of cell-free hemoglobin as a biomarker that could be tested when patients are first admitted to the hospital would be a breakthrough, because it could help quickly determine which patients with sepsis might benefit from acetaminophen therapy.
“One problem in critical care is the patients get sick so fast, that we do not normally have time to figure out which biomarkers help predict which therapy could give the best outcome,” said Michael Matthay, M.D., professor of medicine and anesthesia at the University of California, San Francisco, and the senior study author. “We hope that these findings will underscore the potential therapeutic value of using a biomarker to help successfully find a treatment that will work when patients need it the most.”
To test the therapeutic potential of acetaminophen more fully in a mid-stage clinical trial, researchers enrolled 447 adults with sepsis and respiratory or circulatory organ dysfunction at 40 U.S. academic hospitals from October 2021 to April 2023. Patients were randomized to receive either acetaminophen or a placebo intravenously every six hours for five days. The researchers then followed the patients for 28 days to see how they fared. They also completed a special analysis using data only from the patients with levels of cell-free hemoglobin above a certain threshold. The team’s primary interest overall was the number of patients who were able to stay alive with no organ support, such as mechanical ventilation or kidney failure treatment.
The researchers found that intravenous acetaminophen was safe for all the sepsis patients, with no difference in liver injury, low blood pressure, or other adverse events compared to the placebo group. Among secondary outcomes, they also found that organ injury was significantly lower in the acetaminophen group, as was the rate of acute respiratory distress syndrome onset within seven days of hospital admission.
When looking more closely at the patients with higher cell-free hemoglobin, the researchers found that just 8% of patients in the acetaminophen group needed assisted ventilation compared to 23% of patients in the placebo group. And after 28 days, 12% of patients in the acetaminophen group had died, compared to 21% in the placebo group, though this finding was not statistically significant.
“While the anticipated effects of acetaminophen therapy were not realized for all sepsis patients, this study shows that it still holds promise for the most critically ill” said James Kiley, Ph.D., director of the Division of Lung Diseases at the National Heart, Lung, and Blood Institute, part of NIH. “Though, more research is needed to uncover the mechanisms and validate these results.”
Ware said the results for the critically ill patients trended in a hopeful direction. She and Matthay plan to conduct a larger clinical trial, likely enrolling those patients primarily with higher cell-free hemoglobin levels.
Funding: This study was supported by NHLBI grants: U01 HL122989, U01 HL122998, U01 HL123004, U01 HL123008, U01 HL123009, U01 HL123010, U01 HL123018, U01 HL123020, U01 HL123022, U01 HL123023, U01 HL123027, U01 HL123031, and U01 HL123033.
About the National Heart, Lung, and Blood Institute (NHLBI): NHLBI is the global leader in conducting and supporting research in heart, lung, and blood diseases and sleep disorders that advances scientific knowledge, improves public health, and saves lives. For more information, visit www.nhlbi.nih.gov.
About the National Institutes of Health (NIH):
NIH, the nation’s medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov.
NIH…Turning Discovery Into Health®
Study
Ware LB, Files DC, Fowler A, et al. Phase 2b Randomized Trial of Acetaminophen for Prevention and Treatment of Organ Dysfunction in Critically Ill Sepsis Patients. JAMA. 2024. doi: 10.1001/jama.2024.8772






Post Comment