For the week ending July 6, positive COVID-19 tests crept up by 0.8 percent, COVID-related emergency room visits jumped by more than 23 percent, and hospitalizations increased by just over 13 percent.
“We’re seeing an anticipated summer bump,” says William Schaffner, MD, an infectious disease specialist and a professor of preventive medicine and health policy at the Vanderbilt University School of Medicine in Nashville, Tennessee. “COVID doesn’t disappear during the summertime the way influenza does. If we look back over our past two years, we’ve had an increase during the summer months. It abates again in the fall, and then you get a real seasonal increase during the winter.”
“COVID figures are trending up due to a constellation of factors, including more people congregating close together, more people traveling, and more people going indoors to escape extreme heat,” says Peter Chin-Hong, MD, an infectious disease specialist and a professor of medicine at the University of California San Francisco School of Medicine.
A new suite of variants and waning vaccine immunity may also be contributing to the problem, adds Dr. Chin-Hong.
The New Ks on the Block and the Rise of LB.1
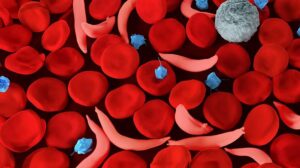
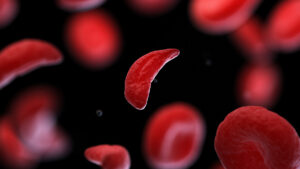
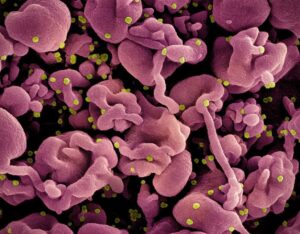
Since COVID-19 initially swept through the world over four years ago, the virus has rapidly mutated. Many versions of the virus have been able to escape the immune defenses people have built up through previous infection or vaccination, although newer versions of COVID-19 haven’t been causing as much serious illness as the versions that occurred early on in the pandemic.
The highly transmissible LB.1 variant is closely related to the FLiRT strains but has an extra mutation. These top four variants are all descendants of the omicron variant JN.1, which now accounts for just over 7 percent of cases but made up more than half of infections at the end of March.
Should You Get a Vaccine Now or Wait?
As the virus quickly changes, vaccine makers are trying to keep up and adjust their formulas to be more effective against circulating strains.
Dr. Schaffner notes that at this point, it is highly unlikely that the fall vaccine can be adjusted any further to directly address a newly rising variant like LB.1. “There is a finite period of time to make these vaccines, get them bottled up, and distribute them,” he says. “The current dominant strains, however, are all subvariants of the omicron family, so the anticipation is that these vaccines for the KP strains will provide antibodies that will protect against LB.1.”
With at least a mini COVID-19 wave happening now, people may wonder if they should wait for the new shots or take further protective action right away.
For Chin-Hong, the answer is pretty straightforward: “Did you get the vaccine approved in the fall of 2023? If not, I would go ahead and get it, especially if you are older than 65 and immunocompromised,” he says. “Those 65 and older can also get another vaccine if four months have elapsed since the last one. That will still give you the ability to get the new vaccine with the flu shot in October or November.”
How Worried Should We Be?
Treatments such as nirmatrelvir and ritonavir (Paxlovid) and remdesivir (Veklury) have also proved to prevent an infection from becoming serious.
“Fortunately, the hospitals have not been overwhelmed as in previous years, attesting to the collective immunity in the population,” says Chin-Hong. “Still, some people are at risk of getting seriously ill: mainly those older than 75 or those who are very immunocompromised who have not gotten the latest vaccine or [been] prescribed Paxlovid or remdesivir when infected.”
Be On the Lookout for COVID-19 Symptoms
Chin-Hong says he’s seeing fewer symptoms that were common in 2020, like shortness of breath and loss of taste and smell, and that some people are experiencing nausea and diarrhea — symptoms they may not realize can be linked to COVID-19.
Because COVID-19 symptoms are often similar to those of allergies (such as hay fever) or the common cold, doctors warn that the only way to know for sure is to take a COVID test — especially if you are vulnerable to severe infection (if you are older, for instance, or are immunocompromised) and want to stave off serious disease with a course of Paxlovid. You should also test if you spend time with anyone at high risk whom you might infect.
Anecdotally, some people on social media are reporting a few fairly nasty effects from the currently circulating virus. A commentator for CNBC recently wrote on X:
“Tested positive for COVID a few days ago. First three days of symptoms were worse than those of 2 years ago. Deep, lingering sore throat among them. Thank goodness for Paxlovid. Seems to be working. Mask up. The new variant appears to be making a bit of a summer surge.”







Post Comment