A new study from scientists at UCLA suggests that maintaining a healthy digestive tract hospitable to “good” bacteria may better equip the brain to deal with the emotional and mental pressures in life.
“When we looked at highly resilient individuals, they had more bacteria related to reduced inflammation and a healthy gut barrier,” says the senior study author, Arpana Gupta, PhD, a codirector of the UCLA Goodman-Luskin Microbiome Center in Los Angeles.
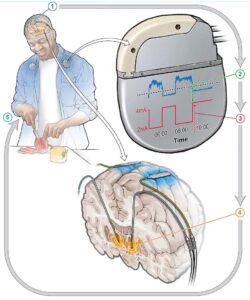
The research, published this month in Nature Mental Health, also showed that resilient people exhibited neural activity in brain regions associated with improved cognition and emotional regulation.
“I think the easiest way to impact your gut microbiome is through diet,” she says, although this study did not look at how diet affects stress. “I believe we can support this gut-brain connection by following a balanced, diverse diet that’s rich in fiber, probiotics, omega-3 fatty acids, and antioxidants, while at the same time minimizing the consumption of highly processed foods, added sugars, artificial sweeteners, and excessive alcohol.”
A Stronger Gut Barrier Is Tied to Stronger Emotional Health
For the study, Gupta and her team surveyed 116 people about their resiliency — such as trust in one’s instincts and positive acceptance of change. Participants were separated into two groups, one for those who ranked high in resiliency and one for those who ranked low.
The researchers took MRI scans of the subjects’ brains to analyze functions related to emotional regulation and cognition. They also collected stool samples to determine what microbes were living in the gut.
Individuals in the highly resilient group indicated that they were less anxious and depressed, and less prone to judgment. They had less perceived stress and less neuroticism, and were less likely to catastrophize and more likely to keep a level head.
MRIs revealed brain activity associated with greater emotional regulation and cognition in the high resiliency group compared with the low resiliency group.
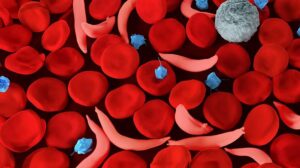
Notably, microbiome activity in the high resiliency group differed from that of the low resiliency group. Mainly, microbiomes in highly resilient individuals excreted metabolites (chemical messengers) and exhibited gene activity associated with therapeutic properties, low inflammation, and a strong gut barrier.
Results suggested that those in the low resilience group were more likely to have a weak gut barrier, otherwise known as a leaky gut. This condition is caused by inflammation and impairs the gut barrier’s ability to absorb essential nutrients while blocking toxins.
“The study goes a long way to establishing a rationale for looking at treating not only psychological difficulties but also GI problems that have been shown to be correlated with psychological stress in a holistic manner,” says Dr. Lupe, who was not involved in the study. “We may start looking at diets that are optimized for gut-microbiome diversity as a treatment for psychological distress as well as physiological functioning.”
A Possible Way to Address Other Stress-Related Health Issues
“Stress is linked to the onset and progression of several diseases,” says Gupta. “If we could increase resilience, then that could help prevent a number of illnesses. Then we’re actually talking about prevention rather than treatment.”
As the study suggests, adopting healthy eating patterns may foster gut health and, in turn, boost resilience to stress. Gupta also emphasizes that working directly on your mental attitude is often key to reducing stress.








Post Comment