The healthcare sector plays a critical role in ensuring the well-being and longevity of individuals. One key aspect that significantly influences healthcare outcomes is the presence of robust healthcare infrastructure. In this article, we will explore the importance of healthcare infrastructure in enhancing access to quality care. We will delve into various aspects such as the definition of healthcare infrastructure, its components, and its impact on healthcare facilities and access. Additionally, we will discuss the pros and cons, alternatives, step-by-step implementation, comparison with other sectors, and provide valuable tips to optimize healthcare infrastructure.
What is Healthcare Infrastructure?
Healthcare infrastructure encompasses the physical and organizational structures that support the delivery of healthcare services. It includes hospitals, clinics, laboratories, medical equipment, information systems, transportation networks, and trained healthcare professionals. A well-developed healthcare infrastructure ensures the availability, accessibility, affordability, and quality of healthcare services.
Components of Healthcare Infrastructure

- Healthcare Facilities: Hospitals, clinics, nursing homes, and diagnostic centers are vital components of healthcare infrastructure. They serve as primary points of contact for individuals seeking medical assistance and play a crucial role in providing comprehensive healthcare services.
- Medical Equipment and Technology: State-of-the-art medical equipment such as MRI machines, surgical robots, and telemedicine tools are integral to modern healthcare infrastructure. These technologies aid in accurate diagnosis, efficient treatment, and remote patient monitoring, improving overall healthcare outcomes.
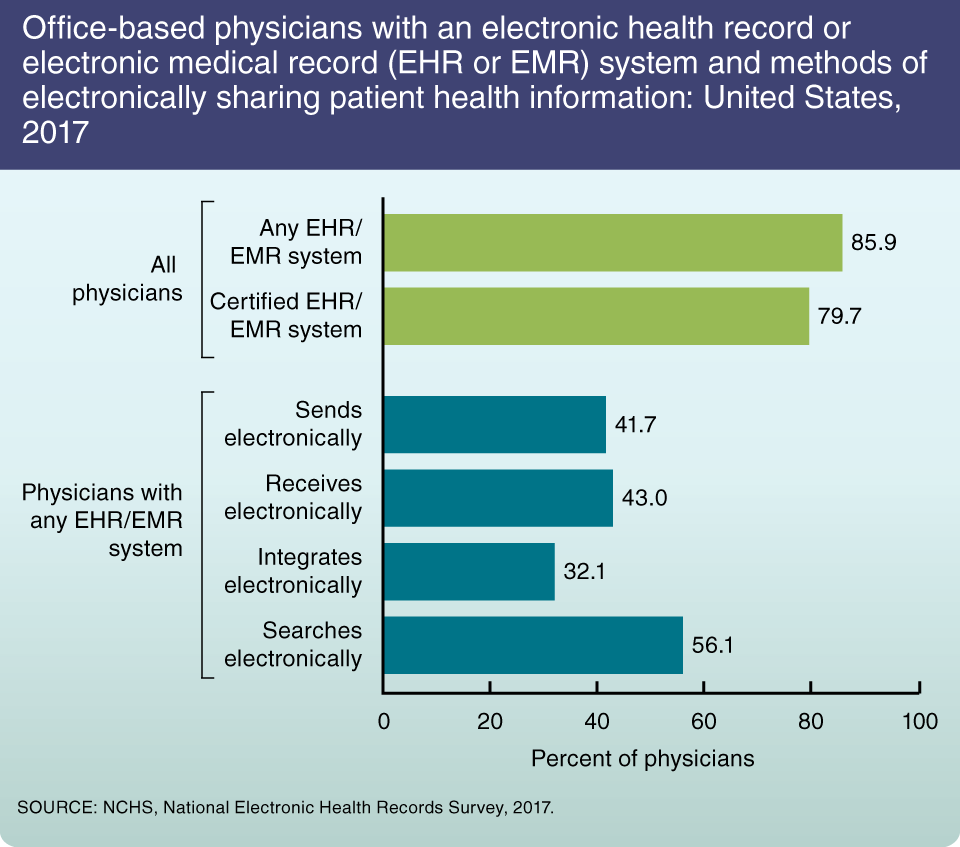
- Health Information Systems: Robust health information systems facilitate the seamless exchange of patient data between healthcare providers, ensuring continuity of care. Electronic health records (EHRs), telehealth platforms, and interoperability standards contribute to effective healthcare information management.
- Trained Healthcare Professionals: Skilled doctors, nurses, technicians, and support staff form the backbone of healthcare infrastructure. Adequate training and continuous professional development programs are essential for maintaining a competent and proficient healthcare workforce.
- Transportation Networks: Accessible transportation networks are crucial for ensuring timely delivery of healthcare services, especially in rural or remote areas. Ambulance services, medical evacuation systems, and well-connected roads contribute to efficient healthcare delivery.
The Impact of Healthcare Infrastructure on Access to Care
Access to quality healthcare is a fundamental right for every individual. Healthcare infrastructure significantly influences this access through several mechanisms:
- Geographical Accessibility: Well-developed healthcare infrastructure ensures that healthcare facilities are geographically distributed to cater to the needs of the population. This reduces travel distances and time, making healthcare services more accessible to individuals living in remote or underserved areas.
*Example*: In rural communities where healthcare infrastructure is limited, individuals often have to travel long distances to reach the nearest hospital. This can lead to delays in accessing timely care, potentially worsening health outcomes. However, with improved healthcare infrastructure, the establishment of smaller satellite clinics or mobile medical units can bring essential healthcare services closer to these communities.
- Affordability: Adequate healthcare infrastructure contributes to cost-effective care by reducing unnecessary expenditures. When healthcare facilities are easily accessible, individuals can seek early preventive measures, reducing the prevalence of advanced diseases that require expensive treatments.
*Example*: A person with diabetes who has access to regular check-ups at a nearby clinic can receive appropriate guidance on managing their condition. This preventive approach helps avoid complications and hospitalizations, ultimately reducing healthcare costs.
- Quality of Care: Healthcare infrastructure enables the provision of high-quality care through well-equipped facilities, skilled professionals, and advanced technologies. This ensures accurate diagnoses, effective treatments, and improved patient outcomes.
*Example*: A well-stocked laboratory equipped with modern diagnostic equipment and trained technicians can provide accurate and timely test results. This leads to precise diagnoses and facilitates appropriate treatment decisions, enhancing patient care.
- Emergency Services: Healthcare infrastructure plays a critical role in delivering emergency medical services promptly. Well-established emergency departments and ambulance networks ensure timely access to life-saving interventions, resulting in better survival rates and improved patient outcomes.
*Example*: In the event of a heart attack, quick access to an emergency department equipped with skilled personnel and appropriate medical equipment increases the chances of successful intervention, minimizing the risk of complications or fatalities.
Pros and Cons of Robust Healthcare Infrastructure
As with any system, there are advantages and disadvantages associated with robust healthcare infrastructure:
Pros
- Improved Health Outcomes: Accessible and well-equipped healthcare facilities contribute to better health outcomes, reducing morbidity and mortality rates.
- Efficient Resource Utilization: An organized healthcare infrastructure optimizes resource allocation, ensuring that facilities, equipment, and personnel are utilized effectively.
- Enhanced Preventive Care: Healthcare infrastructure facilitates preventive care programs, leading to early detection and management of diseases, ultimately reducing healthcare costs.
Cons
- High Initial Costs: Developing and maintaining a sophisticated healthcare infrastructure requires significant financial investments, which can pose challenges for countries with limited resources.
- Maintenanceand Upkeep: Healthcare infrastructure requires regular maintenance and upgrades to keep up with evolving technology and changing healthcare needs. This ongoing cost can strain budgets if not properly managed.
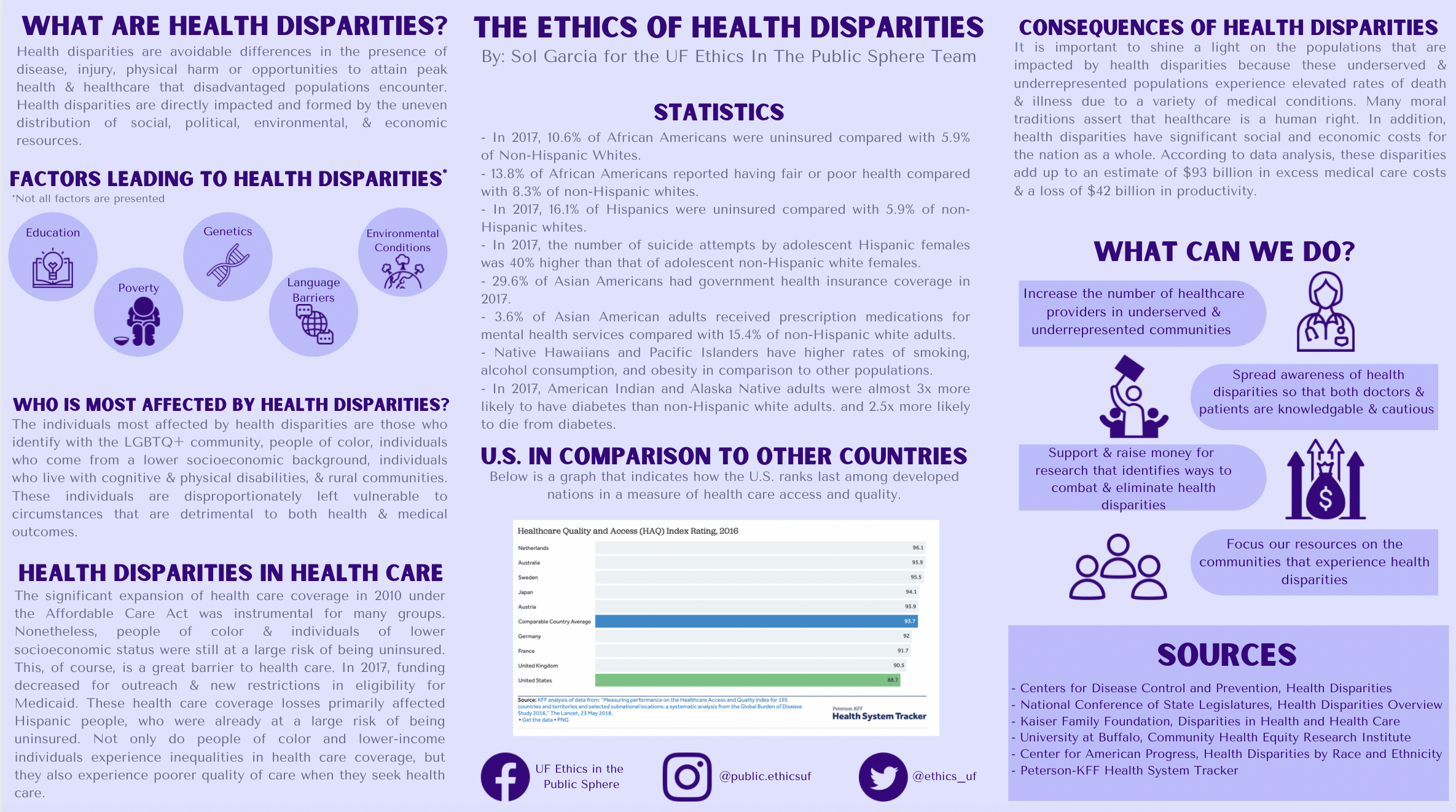
- Disparities in Access: In regions where healthcare infrastructure is unevenly distributed, certain populations may face barriers to accessing quality care, exacerbating health inequities.
Despite the challenges, the benefits of robust healthcare infrastructure outweigh the drawbacks, as it leads to improved healthcare outcomes and overall population health.
Alternatives to Traditional Healthcare Infrastructure
In addition to traditional healthcare infrastructure, there are alternative models that aim to enhance access to quality care:
- Telemedicine: Telemedicine leverages technology to provide remote healthcare services, eliminating geographical barriers and improving access for individuals in remote or underserved areas. It enables virtual consultations, remote monitoring, and access to specialist expertise.
- Community Health Workers: Community health workers act as frontline healthcare providers, especially in resource-constrained settings. They bridge gaps in healthcare access by delivering basic healthcare services, health education, and facilitating referrals.
- Mobile Clinics: Mobile clinics bring healthcare services directly to communities, particularly in rural or hard-to-reach areas. These clinics are equipped with essential medical equipment and staffed by healthcare professionals who provide a range of primary care services.
- Public-Private Partnerships: Collaborations between public and private sectors can help expand healthcare infrastructure. Governments can leverage private sector resources and expertise to build and manage healthcare facilities, improving access and service delivery.
Step-by-Step Guide to Enhancing Healthcare Infrastructure
Improving healthcare infrastructure requires careful planning and implementation. Here’s a step-by-step guide to enhancing healthcare infrastructure:
Step 1: Needs Assessment: Conduct a comprehensive assessment of the existing healthcare infrastructure, identifying gaps, and areas that require improvement. Consider factors such as population demographics, geographic distribution, and specific healthcare needs.
Step 2: Resource Allocation: Allocate resources based on the identified needs. This includes financial investments, healthcare personnel recruitment and training, infrastructure development, and procurement of medical equipment and technology.
Step 3: Infrastructure Development: Construct new healthcare facilities or expand existing ones to meet the growing demand for healthcare services. Ensure that they are well-equipped with appropriate medical technologies and adhere to safety and quality standards.
Step 4: Workforce Development: Invest in healthcare workforce training and professional development programs to ensure a skilled and competent workforce. Recruit and retain healthcare professionals by offering competitive salaries, incentives, and career advancement opportunities.
Step 5: Technological Integration: Incorporate digital health solutions and information systems into healthcare infrastructure to improve efficiency, patient data management, and access to telemedicine services.
Step 6: Collaboration and Partnerships: Foster collaborations and partnerships between healthcare providers, government agencies, private sector entities, and community organizations to ensure comprehensive and coordinated service delivery.
Step 7: Monitoring and Evaluation: Regularly monitor and evaluate the effectiveness of healthcare infrastructure interventions. Collect data on key performance indicators, patient satisfaction, and health outcomes to identify areas for improvement and make evidence-based decisions.
Comparison with Other Sectors
When comparing healthcare infrastructure with other sectors, several key differences and similarities emerge:
- Transportation Infrastructure: While both healthcare and transportation infrastructure aim to improve accessibility, the focus and nature of their operations differ. Healthcare infrastructure focuses on delivering essential medical services, while transportation infrastructure ensures efficient movement of people and goods.
- Information Technology Infrastructure: Healthcare infrastructure incorporates information technology systems to manage patient data, facilitate communication, and improve service delivery. Information technology infrastructure, on the other hand, focuses on providing IT services and connectivity.
- Education Infrastructure: Education infrastructure aims to provide learning environments, while healthcare infrastructure focuses on creating spaces for medical care. Both sectors share the goal of improving human well-being and societal development.
Tips for Optimizing Healthcare Infrastructure
To optimize healthcare infrastructure and enhance access to quality care, consider the following tips:
- Invest in Prevention: Prioritize preventive healthcare measures to reduce the burden of advanced diseases and minimize healthcare costs in the long run.
- Promote Interoperability: Ensure that health information systems and electronic health records are interoperable to facilitate seamless exchange of patient data between healthcare providers.
- Embrace Telemedicine: Leverage telemedicine technologies to overcome geographical barriers, improve access to specialized care, and enable remote monitoring of patients with chronic conditions.
- Empower Community Engagement: Involve communities in healthcare planning and decision-making processes to ensure that healthcare infrastructure aligns with their specific needs and preferences.
- Continuous Quality Improvement: Implement mechanisms for continuous monitoring and evaluation of healthcare infrastructure performance, allowing for ongoing improvements and adjustments based on identified areas of enhancement.
Conclusion
Healthcare infrastructure is an essential component of a well-functioning healthcare system. It plays a vital role in enhancing access to quality care by ensuring geographic accessibility, affordability, and the provision of essential medical services. Robust healthcareinfrastructure encompasses healthcare facilities, medical equipment and technology, health information systems, trained healthcare professionals, and transportation networks. It positively impacts access to care by improving geographical accessibility, affordability, quality of care, and emergency services.
While there are challenges such as high initial costs and maintenance requirements, the benefits of robust healthcare infrastructure outweigh the drawbacks. Alternative models like telemedicine, community health workers, mobile clinics, and public-private partnerships can complement traditional infrastructure and enhance access to care.
Implementing a step-by-step approach, including needs assessment, resource allocation, infrastructure development, workforce training, technological integration, collaboration, and monitoring, can effectively enhance healthcare infrastructure.
When compared to other sectors like transportation infrastructure, information technology infrastructure, and education infrastructure, healthcare infrastructure has unique goals and focuses on delivering essential medical services.
To optimize healthcare infrastructure, investing in prevention, promoting interoperability, embracing telemedicine, empowering community engagement, and implementing continuous quality improvement measures are crucial.
In conclusion, healthcare infrastructure plays a pivotal role in ensuring access to quality care. By addressing geographic barriers, enhancing affordability, and providing necessary resources, it significantly contributes to improved health outcomes and overall population health. Through strategic planning and implementation, healthcare systems can build robust infrastructure to meet the evolving healthcare needs of individuals and communities.
FAQs (Frequently Asked Questions)
1. How does healthcare infrastructure impact healthcare quality?
Robust healthcare infrastructure ensures the availability of well-equipped facilities, advanced technologies, and skilled healthcare professionals, resulting in accurate diagnoses, effective treatments, and improved patient outcomes.
2. What are the challenges of developing healthcare infrastructure?
Developing healthcare infrastructure can be costly, requiring significant financial investments. Additionally, ongoing maintenance and upgrades are necessary to keep up with evolving technology and changing healthcare needs.
3. How can telemedicine contribute to healthcare infrastructure?
Telemedicine leverages technology to provide remote healthcare services, eliminating geographical barriers and improving access for individuals in remote or underserved areas. It enables virtual consultations, remote monitoring, and access to specialist expertise.
4. What role does community engagement play in optimizing healthcare infrastructure?
Involving communities in healthcare planning and decision-making processes ensures that healthcare infrastructure aligns with their specific needs and preferences. This approach leads to more effective and tailored healthcare services.
5. How can continuous quality improvement enhance healthcare infrastructure?
Continuous monitoring and evaluation of healthcare infrastructure performance allow for ongoing improvements and adjustments based on identified areas of enhancement. This ensures that the infrastructure remains efficient, effective, and responsive to changing healthcare demands.




